Premalignant Oral LesionsA routine part of an oral examination should be inspection not only of the teeth and gums but also of the soft tissues in and around the mouth. Dentists look for abnormal changes that are loosely called “lesions.” Many lesions are innocuous and can be easily diagnosed and named based upon their appearance alone. However, some lesions are not as easy to identify and require additional diagnostic steps, such as a biopsy (removal of a piece of the lesion to examine under a microscope). A small percentage of these lesions may be premalignant or even malignant (see education sheet on Oral & Oropharyngeal Cancer). What are these? Premalignant or precancerous (also referred to as “potentially malignant”) oral lesions involve the skin lining of the mouth (known as the epithelium) and may be at risk for becoming (transforming into) an oral cancer, although it is difficult to predict which lesions will transform and how long it will take (see below). Who is at risk for these? As we grow older our risk of developing cancer increases. The same is true for premalignant lesions. Most lesions are detected in people over the age of 40 and those with similar risk factors for oral cancer, such as tobacco and/or heavy alcohol use, although such lesions can also be found in younger individuals and/or those without classic risk factors. How are oral lesions detected? Premalignant lesions and early cancers are usually asymptomatic (ie the patient has no pain and they don’t even know they have a lesion), so their detection is contingent upon a careful soft tissue examination by a dentist. This examination must include the inside and outside of the lips, the cheeks (buccal mucosa), the sides and undersurface of the tongue, the floor of mouth, the gums, the roof of the mouth (palate), the back of the mouth/top of the throat (oropharynx). Most oral lesions are traumatic in nature and have no potential for cancer (Figure A). However, some oral lesions have an appearance which may raise suspicion by the dentist.
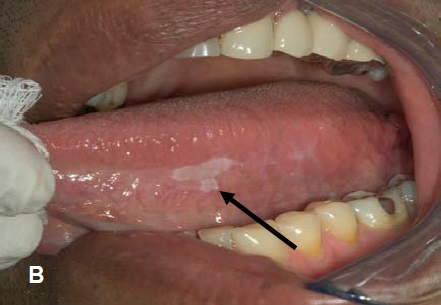
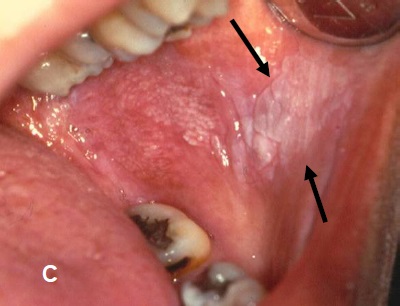
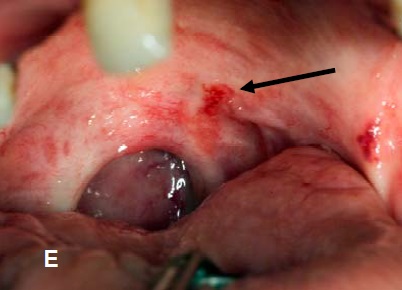
Which lesions might raise suspicion? Patches that are, red, white or mixed red/white in color, or that may also be ulcerated (ie an area where the lining epithelium is lost), especially when found on “high-risk” sites such as the side (lateral surface), underside of the tongue (ventral surface), floor of mouth, or at the back of mouth/top of the throat (oropharynx). A white patch that cannot be wiped off with gauze and for which an explanation is not obvious to the dentist may be defined as a leukoplakia (Figure B & C next page). Similarly, reddish patches with no obvious cause can be defined as erythroplakia (Figure D next page) and mixed red and white areas termed erythroleukoplakia (Figure E next page). Lesions with a red component carry the highest potential for being premalignant or becoming malignant. Some dentists use additional technologies to look for or characterize suspicious lesions (known as diagnostic adjuncts). It is essential to establish an accurate diagnosis for all such lesions that raise suspicion.
What are the possible outcomes of the biopsy? There are three possible outcomes: benign (most frequently), premalignant, or cancer. The pathology report will use pathologic diagnoses such as epithelial hyperplasia/hyperkeratosis or other benign diagnoses, epithelial dysplasia (for premalignant lesions), or squamous cell carcinoma (the most common type of cancer seen in the oral cavity). In epithelial dysplasia, the cells making up the layers of the epithelium look abnormal (atypia), and depending on the amount of abnormal cells seen microscopically, dysplasia may be graded as mild, moderate, severe, or carcinoma in situ (where the atypical cells are in all layers of the epithelium). In squamous cell carcinoma these abnormal cells are no longer confined just to the epithelium but have invaded below the epithelium into deeper tissues. How are patients with oral epithelial dysplasia managed? Patients with high-grade dysplasia (severe or carcinoma-in-situ) generally have a higher chance for malignant transformation than those with lower-grade dysplasias. It is extremely important that patients with oral epithelial dysplasia be followed by a specialist who is trained to manage these types of lesions. Eliminating high-risk behaviors and promoting protective behaviors (such as a healthy diet) are essential. Surgical removal of a premalignant lesion may or may not be warranted. Regardless of removal, periodic close follow-up of the patient for any visual changes to the lesion site is critical because lesions can recur and transformation into a malignant lesion is possible at anytime. QUESTIONS AND ANSWERS ABOUT PREMALIGNANT ORAL LESION Q: My dentist said I have a dysplasia, what does it mean? Q: I have a premalignant lesion on the tongue will this spread to other parts of my mouth or body? Q: If I quit smoking, will the lesions disappear? Q: Are biopsies complicated or painful? Q: If the lesion was removed, do I still need to see my dentist? Q: My dentist has a new device for detecting lesions. Is this really necessary or better than a regular exam? Q: Does dysplasia mean I am going eventually to develop cancer? NOTE: Lesions on the lips that result from sun exposure (solar cheilitis) are also premalignant lesions (see PATIENT INFORMATION SHEET: Lip Changes - Solar Cheilitis). Recommended Links: Prepared by R Czerninski, D Lederman, H Ephros, and R Kerr The information contained in this monograph is for educational purposes only. This information is not a substitute for professional medical advice, diagnosis, or treatment. If you have or suspect you may have a health concern, consult your professional health care provider. Reliance on any information provided in this monograph is solely at your own risk. |